
Gene Therapy Center Developing Cutting-Edge Treatments
Precision medicine, an approach that uses information about an individual’s unique variations to treat or prevent disease, is changing the future of medicine.
Rather than tackling symptoms, precision medicine — sometimes called personalized or individualized medicine — looks at the root cause of illnesses. Some of the information used to determine treatment can include genetic variations and mutations, lifestyle, the environment, or even a person’s unique microbiome.
Personalized medicine is not new, but research momentum for individualized cures is growing.
Close to half of the new molecular entities approved by the FDA in 2018 are considered personalized or precision medicine treatments.
A report by BIS Research estimated the precision medicine market at around $79 billion in 2018, and expects it to grow to more than $216 billion by 2028. Companies involved in developing precision medicine treatments include Roche, Novartis, Pfizer and other industry icons.
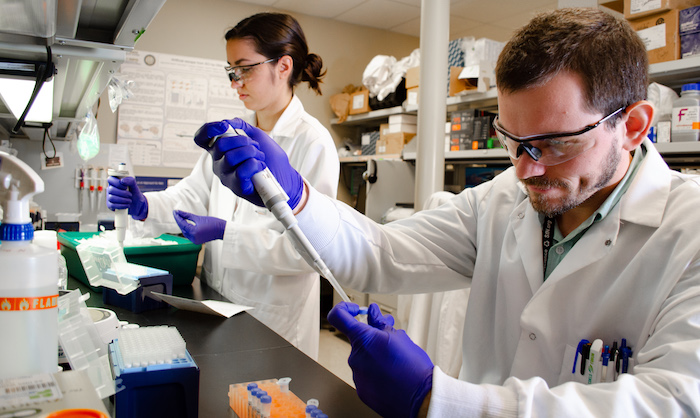
Gene therapy is one type of precision medicine that uses several mechanisms to insert a gene into a patient’s cells to treat medical disorders caused by mutated, defective or missing genes.
Gene-editing technologies including CRISPR-Cas9 and other techniques, can allow scientists to alter, add, or remove parts of a genome.The experimental therapy can replace a disease-causing gene with a healthy copy, inactivate a malfunctioning gene, or introduce a new gene to help fight disease.
Scientists use what are called “vectors” to insert the new genes directly into cells. Viruses, for example, can be modified so they do not cause infectious diseases, but instead carry therapeutic genes that deliver the desired genetic material into cells. Multiple types of stem cells, including those from a patient, also can be vectors that deliver genetic material targeted at treating various diseases.
Gene therapy is being explored for the treatment not only of inherited disorders but also a variety of other diseases, including cancer, rheumatoid arthritis, diabetes, Parkinson’s disease and Alzheimer’s disease.
Gene therapy research at UC Davis
UC Davis’ commitment to stem cell and gene therapy research dates back more than a decade.
In 2010, with major support from the California Institute for Regenerative Medicine (CIRM), UC Davis launched the UC Davis Institute for Regenerative Cures, which includes research facilities as well as a Good Manufacturing Practice (GMP) facility.
In 2016, led by Fred Meyers, a professor in the School of Medicine, UC Davis launched the Center for Precision Medicine and Data Sciences, bringing together innovations such as genomics and biomedical data sciences to create individualized treatments for patients.
Last year, the university launched the Gene Therapy Center, part of the IMPACT Center program.
Led by Jan Nolta, a professor of cell biology and human anatomy and the director of the UC Davis Institute for Regenerative Cures, the new center leverages UC Davis’ network of expert researchers, facilities and equipment to establish a center of excellence aimed at developing lifelong cures for diseases.
Nolta began her career at the University of Southern California working with Donald B. Kohn on a cure for bubble baby disease, a condition in which babies are born without an immune system. The blood stem cell gene therapy has cured more than 50 babies to date.
Work at the UC Davis Gene Therapy Center targets disorders that potentially can be treated through gene replacement, editing or augmentation.
“The sectors that make up the core of our center stretch out across campus,” said Nolta. “We work with the MIND Institute a lot. We work with the bioengineering and genetics departments, and with the Cancer Center and the Center for Precision Medicine and Data Sciences.”
A recent UC Davis stem cell study shows a potential breakthrough for healing diabetic foot ulcers with a bioengineered scaffold made up of human mesenchymal stem cells (MSCs). Another recent study revealed that blocking an enzyme linked with inflammation enables stem cells to repair damaged heart tissue. A cell gene therapy study demonstrated restored enzyme activity in Tay-Sachs disease affected cells in humanized mouse models.

Several cell and gene therapies have progressed to the point that ongoing clinical trials are being conducted at UC Davis for diseases, including sickle-cell anemia, retinopathy, muscle injury, dysphasia, advanced cancer, and Duchenne muscular dystrophy, among others.
“Some promising and exciting research right now at the Gene Therapy Center comes from work with hematopoietic stem cells and with viral vector delivery,” said Nolta.
Hematopoietic stem cells give rise to other blood cells. A multi-institutional Phase I clinical trial using hematopoietic stem cells to treat HIV-lymphoma patients is currently underway at UC Davis.

“We are genetically engineering a patient’s own blood stem cells with genes that block HIV infection,” said Joseph Anderson, an associate professor in the UC Davis Department of Internal Medicine. The clinical trial is a collaboration with Mehrdad Abedi, the lead principal investigator.
“When the patients receive the modified stem cells, any new immune system cell, like T-cell or macrophage, that is derived from one of these stem cells, will contain the HIV-resistant genes and block further infection,” said Anderson.
He explained that an added benefit with the unique therapy is that it contains an additional gene that “tags” the stem cells. “We are able to purify the HIV-resistant cells prior to transplantation, thus enriching for a more protective cell population.”
Kyle David Fink, an assistant professor of neurology at UC Davis, is affiliated with the Stem Cell Program and Institute for Regenerative Cures. His lab is focused on leveraging institutional expertise to bring curative therapies to rare, genetically linked neurological disorders.
“We are developing novel therapeutics targeted to the underlying genetic condition for diseases such as CDKL5 deficiency disorder, Angelman, Jordan and Rett syndromes, and Juvenile Huntington’s disease,” said Fink.
The lab is developing therapies to target the underlying genetic condition using DNA-binding domains to modify gene expression in therapeutically relevant ways. They are also creating novel delivery platforms to allow these therapeutics to reach their intended target: the brain.
“The hope is that these highly innovative methods will speed up the progress of bringing therapies to these rare neurodegenerative disease communities,” said Fink.

Developing potential lifetime cures
Among Nolta’s concerns is how expensive gene therapy treatments can be.
“Some of the therapies cost half a million dollars and that’s simply not available to everyone. If you are someone with no insurance or someone on Medicare, which reimburses about 65 percent, it’s harder for you to get these life-saving therapies,” said Nolta.
To help address that for cancer patients at UC Davis, Nolta has set up a team known as the “CAR T Team.”
Chimeric antigen receptor (CAR) T-cell therapy is a type of immunotherapy in which a patient’s own immune cells are reprogrammed to attack a specific protein found in cancer cells.
“We can develop our own homegrown CAR T-cells,” said Nolta. “We can use our own good manufacturing facility to genetically engineer treatments specifically for our UC Davis patients.”
Although safely developing stem cell treatments can be painfully slow for patients and their families hoping for cures, Nolta sees progress every day. She envisions a time when gene therapy treatments are no longer considered experimental and doctors will simply be able to prescribe them to their patients.
“And the beauty of the therapy is that it can work for the lifetime of a patient,” said Nolta.
Article originally published by UC Davis Office of Research.
Media Resources
Media Contact(s)
- AJ Cheline, Office of Research, 530-752-1101, acheline@ucdavis.edu
- Jan Nolta, Institute for Regenerative Cures, janolta@ucdavis.edu
Resources